Colposcopy & Urodynamics Clinic for Women
Colposcopy
What is colposcopy?
Colposcopy is a procedure in which a special magnifying instrument called a colposcope is used to look into the vagina and into the cervix. The colposcope gives an enlarged view of the outer portion of the cervix.
Why would a colposcopy be necessary?
Colposcopy is done when there are abnormal changes in the cells of the cervix as seen on a Pap test. Further, it may be done to assess problems such as genital warts on the cervix, inflammation of the cervix, benign growths or polyps, pain and bleeding.
How is the procedure done?
During a colposcopy, you will lie on your back with feet raised just as you do when you have a regular pelvic exam. The doctor uses an instrument called a speculum to hold the walls of the vagina apart. Then the colposcope is placed at the opening of your vagina. A mild solution may be applied to the vagina and cervix with a cotton swab. This makes abnormal areas to be seen easily. The doctor will look inside the vagina to locate any problem. If there are any abnormalities, the doctor may take a small tissue sample called a biopsy. You may feel a mild pinch or cramp while the biopsy sample is taken. The tissue is then sent to a laboratory for further study.
What to expect after the procedure?
Your gynaecologist will talk to you about any problems detected during colposcopy. If a sample of tissue was taken from your cervix (biopsy), the laboratory results should be ready in 2 to 3 weeks.
Most women feel fine after colposcopy. You may feel a little lightheaded and if you had a biopsy, you may have some mild bleeding. Talk to your gynaecologist about how to take care of yourself after the procedure and when you need to return for a check-up.
What are the risks of colposcopy?
There may be a risk of infection when you have a colposcopy. Mild pain and cramping during the procedure and mild bleeding afterwards are common. This most often happens when a biopsy is done. If there is heavy bleeding, fever, or severe pain after the procedure, contact your gynaecologist immediately.
Colposcopy is used to look for problem cells when a pap smear has reported an abnormality. A digital, video colposcope allows problem areas that may be invisible to the naked eye, to be seen. A vinegar-like solution (acetic acid) is sometimes used to make areas of abnormality easier to see clearly and a sample of tissue may be taken (biopsy) to test for abnormal cells. Biopsy results will be available one week after the procedure.
Urodynamics
Urodynamics testing is used to assess and diagnose the cause of many common bladder problems, including incontinence. Studies by The Australian Institute of Health and Welfare (2006) found that 37% of Australian woman have been affected by urinary incontinence, while other studies put the figure even higher. These problems are often due to the effects of child-bearing or hormonal changes at menopause. Modern treatments are effective, and the outcome of the urodynamics test will determine the most appropriate treatment option for each individual. We will provide you with specific information brochures for your recommended treatment options.
A typical study takes about 30 minutes and involves the use of a small catheter to fill the bladder. Several measurements of volume and pressure are recorded. You might experience some discomfort when passing urine for 24 hours after the procedure, but this should settle quickly. Ensuring you drink plenty of fluids during this time will ease your discomfort. Please contact Dr Gailani if you are concerned.
If you have a problem with urine leakage or blocked urine flow, your doctor may be able to help. One of the tools they may use to evaluate the cause of your symptoms is urodynamic testing.
Several muscles, organs, and nerves are involved in collecting, storing, and releasing urine. The kidneys form urine by filtering wastes and extra water from the bloodstream. The ureters are tubes that carry urine from the kidneys to the bladder. Normally urine flows in one direction. If urine backs up toward the kidneys, infections and kidney damage can occur.
The bladder, a hollow muscular organ shaped like a balloon, sits in the pelvis and is held in place by ligaments attached to other organs and to the pelvic bones. The bladder stores urine until you are ready to empty it. It swells into a round shape when it is full and gets smaller as it empties. A healthy bladder can hold up to 500ml of urine comfortably. How frequently it fills depends on how much excess water your body is trying to get rid of.
The bladder opens into the urethra, the tube that allows urine to pass outside the body. Circular muscles called sphincters close tightly to keep urine from leaking. The involuntary leakage of urine is called incontinence.
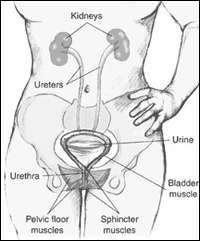
Nerves in the bladder tell you when it is time to empty your bladder. When the bladder begins to fill with urine, you may notice a feeling that you need to urinate. The sensation becomes stronger as the bladder continues to fill and reaches its limit. At that point, nerves in the bladder send a message to the brain, and your urge to urinate intensifies.
When you are ready to urinate, the brain signals the sphincter muscles to relax. At the same time, the brain signals the bladder muscles to squeeze, thus allowing urine to flow through the urethra. When these signals occur in the correct order, normal urination occurs.
Problems in the urinary system can be caused by aging, illness, or injury. The muscles in and around your bladder and urethra tend to become weaker with age. Weak bladder muscles may result in your not being able to empty your bladder completely, leaving you at a higher risk for urinary tract infections. Weak muscles of the sphincters and pelvis can lead to urinary incontinence because the sphincter muscles cannot remain tight enough to hold urine in the bladder, or the bladder does not have enough support from the pelvic muscles to stay in its proper position.
Urodynamic is a study that assesses how the bladder and urethra are performing their job of storing and releasing urine. Urodynamic tests help your doctor see how well your bladder and sphincter muscles work and can help explain symptoms such as
- Incontinence
- Frequent urination
- Sudden, strong urges to urinate
- Problems starting a urine stream
- Painful urination
- Problems emptying your bladder completely
- Recurrent urinary tract infections
Seeing Your Doctor or Nurse
The first step in solving a urinary problem is to talk with your doctor. He or she should ask you about your general medical history, including any major illnesses or surgeries. You should talk about the medicines you take, both prescription and non-prescription, because they might be part of the problem. You should talk about how much fluid you drink a day and whether you use alcohol or caffeine. Give as many details as you can about the problem and when it started. The doctor or nurse may ask you to keep a voiding diary, which is a record of fluid intake and trips to the bathroom, plus any episodes of leakage
If leakage is the problem, the doctor may ask you to do a pad test. This test is a simple way to measure how much urine leaks out. You need to weight a dry pad you normally use and put all the used pads into a plastic bag to weigh them at the end of the 24-hour period.
A physical exam will also be performed to rule out other causes of urinary problems. This exam usually includes an assessment of the nerves in the lower part of your body. It will also include a pelvic exam in women to assess the pelvic muscles and the other pelvic organs. In men, a rectal exam is given to assess the prostate. Your doctor will also want to check your urine for evidence of infection or blood.
Preparing for the Test
If the doctor recommends bladder testing, usually no special preparations are needed, but make sure you understand any instructions you do receive.
Taking the Test
Most urodynamic testing focuses on the bladder's ability to empty steadily and completely. It can also show whether the bladder is having abnormal contractions that cause leakage. Your doctor will want to know whether you have difficulty starting a urine stream, how hard you have to strain to maintain it, whether the stream is interrupted, and whether any urine is left in your bladder when you are done. The remaining urine is called the postvoid residual.
Uroflowmetry (Measurement of Urine Speed and Volume)
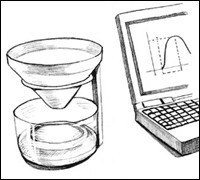
A uroflowmeter automatically measures the amount of urine and the flow rate-that is, how fast the urine comes out. You may be asked to urinate privately into a toilet that contains a collection device and scale. This equipment creates a graph that shows changes in flow rate from second to second so the doctor can see the peak flow rate and how many seconds it took to get there. Results of this test will be abnormal if the bladder muscle is weak or urine flow is obstructed.
Measurement of Postvoid Residual
After you have finished, you may still have some urine remaining in your bladder. Postvoid residual can be measured with ultrasound equipment that uses harmless sound waves to create a picture of the bladder. The amount of postvoid residual can be different each time you urinate.
Cystometry (Measurement of Bladder Pressure)
A cystometrogram (CMG) measures how much your bladder can hold, how much pressure builds up inside your bladder as it stores urine, and how full it is when you feel the urge to urinate. Two catheters are inserted into the bladder via the urethra, one to fill the bladder with fluid and another to measure pressure. Another catheter may be placed in the rectum to record pressure there as well. Your bladder will be filled slowly with water. During this time you will be asked how your bladder feels and when you feel the need to urinate. The volume of water and the bladder pressure will be recorded. You may be asked to cough or strain during this procedure. Involuntary bladder contractions can be identified.
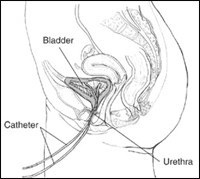
Measurement of Leak Point Pressure
While your bladder is being filled for the CMG, it may suddenly contract and squeeze some water out without warning. The manometer will record the pressure at the point when the leakage occurred. This reading may provide information about the kind of bladder problem you have. You may also be asked to apply abdominal pressure to the bladder by coughing, shifting position, or trying to exhale while holding your nose and mouth. These actions help the doctor evaluate your sphincter muscles.
Pressure Flow Study
After the CMG, you will be asked to empty your bladder. The catheter can measure the bladder pressures required to urinate and the flow rate a given pressure generates. This pressure flow study helps to identify bladder outlet obstruction that men may experience with prostate enlargement. Bladder outlet obstruction is less common in women but can occur with a fallen bladder or rarely after a surgical procedure for urinary incontinence.
Electromyography (Measurement of Nerve Impulses)
If your doctor thinks that your urinary problem is related to nerve or muscle damage, you may be given an electromyography. This test measures the muscle activity in and around the urethral sphincter by using special sensors. The sensors are placed on the skin near the urethra. Muscle activity is recorded on a machine. The patterns of the impulses will show whether the messages sent to the bladder and urethra are coordinated correctly.
Video Urodynamic Study
Urodynamic tests may be performed with or without equipment to take pictures of the bladder during filling and emptying. The imaging equipment may use x rays or sound waves. If x-ray equipment is used, the bladder will be filled with a contrast medium that will show up on the x-ray. The pictures and videos show the size and shape of the urinary tract and help your doctor understand your problem.
After the Test
You may have mild discomfort for a few hours after these tests when you urinate. Drinking a glass of water each half-hour for 2 hours should help.
If you have signs of infection including pain, chills, or fever contact your specialist or family doctor.
Getting the Results
Results for simple tests can be discussed with your doctor immediately after the test. Results of other tests may take a few days. You will have the chance to ask questions about the results and possible treatments for your problem.
MedGyn Digital Video Colposcope
MedGyn Digital Video Colposcope and Image Management System
Device Description
Different from the traditional optical colposcope, this colposcope’s innovative LED light source ensures high brightness with a long life cycle. Its light spot subtraction technology and unique CCD/optics design provide high-definition images and improved viewing of blood vessels, capturing every meticulous detail.